A 55-year-old woman is brought to the emergency department due to a sudden onset of retrosternal chest pain. An ECG shows ST-segment elevation. A diagnosis of myocardial infarction is made and later confirmed by elevated levels of troponin I. The patient is sent to the cardiac catheter laboratory to undergo percutaneous catheterization. She has 2 occluded vessels in the heart. The patient undergoes percutaneous coronary intervention to implant 2 stents in her coronary arteries, and the blood flow is successfully restored in the affected arteries. The patient complains of flank pain during post-procedure evaluation a few hours later. A significant drop in hematocrit is observed, as well as a decline in her blood pressure to 90/60 mm Hg. Physical examination reveals extensive ecchymoses in the flanks and loin as shown in the image. Which of the following conditions is this patient most likely experiencing?
A. Complication from femoral artery access
B. Fat embolism
C. Patent ductus arteriosus
D. Adrenal hemorrhage
E. Ventricular septal defect
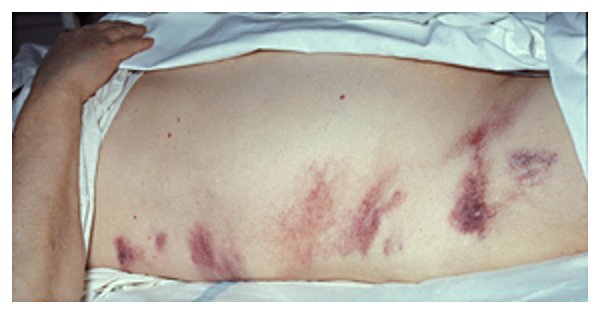
Image by Herbert L. Fred, MD and Hendrik A. van ****. License: CC BY 2.0